Why do you need my data? A co-creative approach to enriching public dialogues around health data
What happens to health data?
Debates about the use of patient data often produce more heat than light. Last year’s failed GP data roll out showed the consequences of policy makers not being upfront about how decisions are made, the choices people have and how public views are built into the process. This episode also highlighted the lack of clear, impartial information out there.
So, the Understanding Patient Data (UPD) team was keen to produce an open, balanced and engaging guide to large-scale patient data sets. Our past engagement work has shown that members of the public ask thoughtful questions about how large-scale health data sets operate, the potential risks and benefits, what safeguards are in place and the trade-offs. We wanted to provide clear, readily available answers to these questions.
A co-creative approach
The idea for this project originated in a conversation with the OpenSAFELY team, who are grantees of our wider Data for Science and Health department at the Wellcome Trust. We then took the idea to a scoping workshop with a group of experts – privacy academics, datahub clinical leads, policy specialists and patient representatives. Their insights were invaluable as we thought through the broad content of the guide and what we should ask for in our commissioning brief. We are very grateful to everyone in the group for the time they gave at the workshop and at later stages when they reviewed the draft guide and contributed to dissemination.
Thanks to the scoping workshop, we had a clear idea of the issues we wanted the guide to cover. We also knew that if we wanted the guide to be well used - it would need to be crisp, accurate and well designed. We put out a request for proposals and were delighted to partner with Open Creative Communications (OCC) on the project. They brought just the clear thinking, design eye and way with words that we were looking for.
At the heart of OCC’s approach, were their co-production workshops in which they tested out content with members of the public. In these sessions, they held quick-fire rounds to select preferred terms, agreed the best order of information and tested out the clarity of the language.
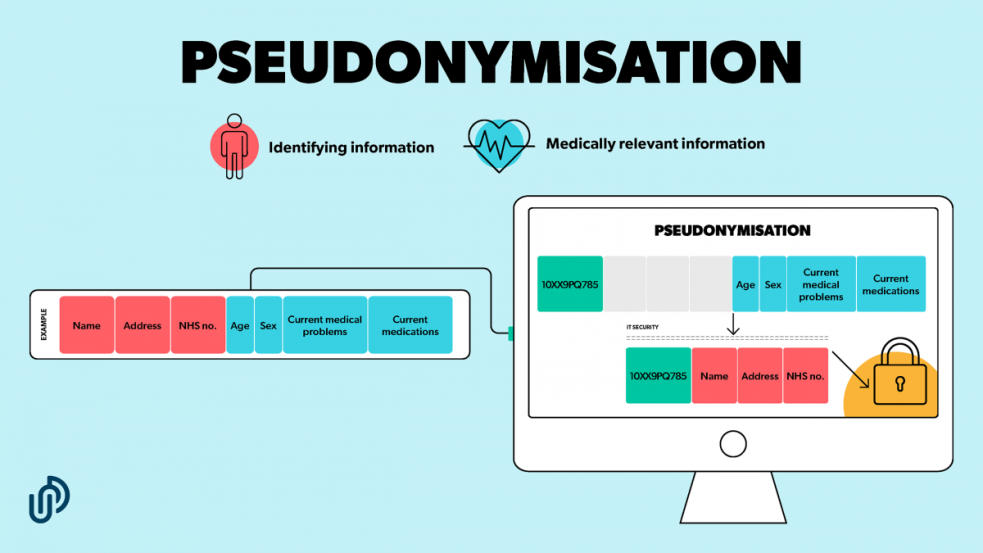
A particular point of confusion in this field is the use of the term ‘pseudonymised’ data. The experts and members of the public in all our workshops agreed that this is an unclear, even misleading, word and a straightforward explanation and visuals were needed. We think this is the first public guide to do so.
Discussions with the advisory group and public workshops highlighted two main challenges. Firstly, getting the balance right between concise yet accurate information – both in the text and through the visuals. Secondly, providing objective information on the risks, benefits and trade-offs when it came to this hotly debated issue.
The finalised guide was entirely reformulated in response to people’s feedback at the public workshops. The National Data Guardian, which exists to ensure citizens’ health information is safeguarded, welcomed the fact that the project ‘involved the public to produce a guide that is clear and easy to follow.’ This work demonstrates how both public and patient involvement and engagement are central to informed public discussion on health.
Making it stick
OCC also went to great lengths to speak to people working in the health service to understand how the guide might be used on the ground. Our aim was not only to produce a guide that accurately and accessibly explained the use of large-scale data sets, but one that could be used in a range of settings by a wide variety of people. In addition to the core guide, OCC produced animations, social media assets a poster for NHS waiting rooms, with a QR code for more information.
The variety of formats, together with the conversations that both OCC and our team had with relevant organisations during the co-production phase, meant that the take up has been excellent. NHS Transformation, the Royal College of GPs and the National Data Guardian are actively sharing the guide. NHS UK plan to take this version and use it in further cocreation work with patients and the public, so they have content that is adapted to their needs.
This guide, like most UPD resources, is published under creative commons and we actively encourage organisations to share our content and tailor it for their audiences.
Our hope is that the next time a debate on health data arises, people -members of the public, health staff, policy makers and journalists - have a useful guide to hand, to support well-informed public debate.
Going further
While it is essential that individual resources are co-produced with the people you hope will use them, we recognise that content-specific collaboration of this kind is not enough on its own. Members of the public should be at the heart of discussion and decision making on health data, on an ongoing and sustainable basis.
We welcome the news that NHS Digital are recruiting a Patient and Public Engagement and Communications Advisory Panel. The panel will advise on the communication and engagement strategy on the GP data initiative, as well as content.
On the face of it, this looks to be a useful response to the hard lessons learned last year. Embedding the role of members of the public must become the norm, so people are able to take a leading role in shaping both specific engagement resources and the broader direction of travel.
Tell us more
We would be keen to hear your thoughts and feedback on the resources we have produced, and would love you to share them and use them in your own work.
We’d also like to know of any other initiatives that aim to embed the perspective of patients and the public – especially those using innovative digital methods to do so. This is a new area of focus for us within Data for Science and Health. Please do get in touch with us at engagement@understandingpatientdata.org.uk if you are involved with, or know of, examples of good and novel practice in the UK or globally.
Download the ‘What happens to Health Data?’ guide
This blog is by Rebecca Asher and Emily Jesper-Mir, Strategy and Engagement Managers (job share), Understanding Patient Data, and freelance policy and public engagement specialists. UPD is currently hosted at Wellcome Trust.
Find out more about the guide and access further digital resources here.